ChatGPT:
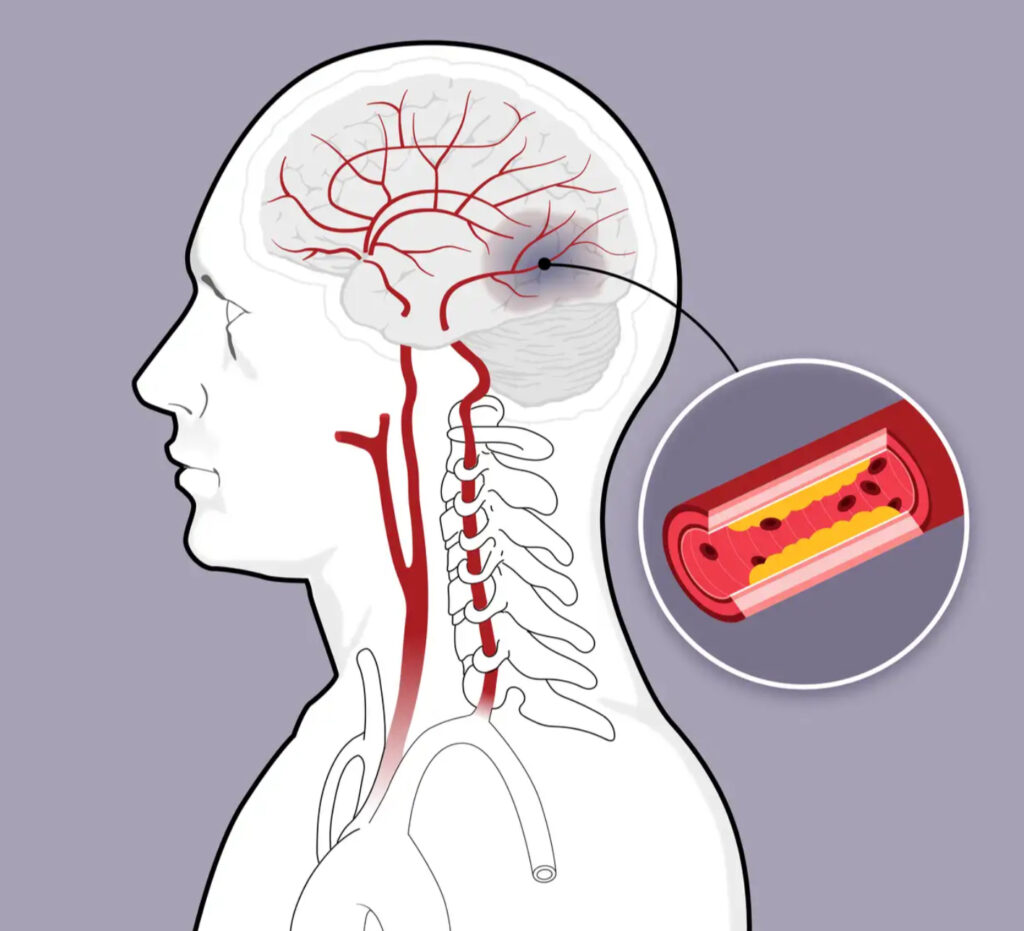
A stroke occurs when the blood supply to a part of the brain is interrupted or reduced, preventing brain tissue from getting enough oxygen and nutrients. This can happen in two main ways:
- Ischemic Stroke: This is the most common type and occurs when a blood clot blocks or narrows an artery leading to the brain.
- Hemorrhagic Stroke: This happens when a blood vessel in the brain bursts, leading to bleeding in or around the brain.
Both types of stroke can cause brain cells to begin dying within minutes. The effects of a stroke can vary depending on the part of the brain affected, but common symptoms include sudden numbness or weakness in the face, arm, or leg (especially on one side of the body), confusion, trouble speaking, difficulty walking, dizziness, and severe headache. Prompt medical attention is crucial to minimize damage and improve recovery chances.
A mini-stroke, medically known as a Transient Ischemic Attack (TIA), occurs when the blood flow to a part of the brain is temporarily blocked or reduced. Unlike a full stroke, the symptoms of a TIA are temporary, usually lasting only a few minutes to a few hours, and they don’t cause permanent damage.
However, a TIA is a serious warning sign that a full stroke might occur in the future. The symptoms of a TIA are similar to those of a stroke, including sudden numbness or weakness in the face, arm, or leg (especially on one side of the body), confusion, trouble speaking, difficulty walking, dizziness, and severe headache.
Because TIAs and strokes share the same symptoms, it’s important to seek immediate medical attention, even if the symptoms go away quickly. Early intervention can help prevent a full stroke and potentially save a life.
Strokes affect the brain by disrupting the flow of blood to specific areas, depriving brain cells of oxygen and essential nutrients. When brain cells don’t get enough oxygen, they begin to die, leading to the loss of functions controlled by that part of the brain. The impact of a stroke on the brain depends on several factors:
- Location of the Stroke:
- Left Hemisphere: Strokes in the left side of the brain can affect language, speech, and the ability to understand language (aphasia). They can also cause right-sided weakness or paralysis and difficulties with reading, writing, and arithmetic.
- Right Hemisphere: Strokes in the right side of the brain can cause left-sided weakness or paralysis. They may also lead to issues with spatial awareness, attention, judgment, and short-term memory.
- Brainstem: If a stroke occurs in the brainstem, it can affect both sides of the body, potentially leading to more severe symptoms such as problems with breathing, heart function, balance, and coordination, or even coma.
- Size of the Stroke:
- Small Stroke: A small stroke might only affect a limited area of the brain, leading to more localized and potentially less severe symptoms.
- Large Stroke: A large stroke can damage a significant portion of the brain, leading to more extensive and severe impairments.
- Type of Stroke:
- Ischemic Stroke: The most common type, caused by a blockage in an artery. The area of the brain affected by the lack of blood flow will determine the symptoms.
- Hemorrhagic Stroke: Caused by a ruptured blood vessel, leading to bleeding in or around the brain. The pressure from the bleeding can further damage brain tissue and lead to more widespread effects.
- Duration of the Stroke:
- The longer the brain is deprived of blood and oxygen, the more extensive the damage. Prompt treatment can minimize the effects and improve the chances of recovery.
Common effects of a stroke on the brain include:
- Motor Impairments: Weakness or paralysis on one side of the body.
- Sensory Issues: Numbness, tingling, or loss of sensation.
- Cognitive Deficits: Memory loss, difficulty with attention, problem-solving, and decision-making.
- Speech and Language Problems: Trouble speaking, understanding language, reading, or writing.
- Emotional and Behavioral Changes: Mood swings, depression, anxiety, and changes in personality.
The brain’s plasticity, or ability to reorganize itself, plays a key role in recovery after a stroke. With therapy and rehabilitation, some functions can be regained or compensated for, depending on the severity and location of the stroke.
Several medical conditions and health problems can significantly increase the risk of having a stroke. Here’s a list of the most common ones:
- High Blood Pressure (Hypertension): The leading risk factor for stroke, high blood pressure can damage blood vessels over time, making them more likely to rupture or become blocked.
- Heart Disease: Conditions like coronary artery disease, heart failure, and valve defects can increase the risk of clots forming in the heart and traveling to the brain, causing a stroke.
- Atrial Fibrillation: This irregular heartbeat can cause blood to pool and form clots in the heart, which can then travel to the brain and lead to a stroke.
- Diabetes: People with diabetes are more likely to have high blood pressure and high cholesterol, both of which increase the risk of stroke. Additionally, diabetes can damage blood vessels, making a stroke more likely.
- High Cholesterol: Elevated levels of cholesterol can lead to the buildup of plaques in the arteries (atherosclerosis), which can block blood flow to the brain.
- Previous Stroke or Transient Ischemic Attack (TIA): A history of stroke or TIA significantly increases the risk of future strokes.
- Obesity: Excess body weight increases the risk of high blood pressure, diabetes, and heart disease, all of which are stroke risk factors.
- Smoking: Smoking damages blood vessels, increases blood pressure, and makes blood more likely to clot, all of which increase stroke risk.
- Excessive Alcohol Consumption: Heavy drinking can raise blood pressure, increase cholesterol levels, and contribute to the development of atrial fibrillation, all of which heighten stroke risk.
- Physical Inactivity: A sedentary lifestyle can lead to obesity, high blood pressure, diabetes, and high cholesterol, which are all risk factors for stroke.
- Sleep Apnea: This sleep disorder, characterized by pauses in breathing during sleep, can lead to high blood pressure and heart problems, increasing stroke risk.
- Carotid Artery Disease: Narrowing of the carotid arteries, which supply blood to the brain, can lead to reduced blood flow and increase the likelihood of a stroke.
- Peripheral Artery Disease (PAD): Similar to carotid artery disease, PAD involves narrowing of the blood vessels, which can reduce blood flow and increase stroke risk.
- Sickle Cell Disease: This genetic condition causes blood cells to form an abnormal shape, which can lead to blockages in blood vessels and increase the risk of stroke.
- Certain Blood Disorders: Conditions like polycythemia, which causes increased red blood cell production, can thicken the blood and make clots more likely, raising the risk of stroke.
- Inflammatory Conditions: Diseases such as lupus and rheumatoid arthritis can cause inflammation in blood vessels, increasing the risk of stroke.
Managing these conditions effectively with the help of healthcare professionals can significantly reduce the risk of stroke.
Diagnosing a stroke quickly and accurately is crucial for effective treatment. The diagnosis typically involves a combination of clinical evaluation, imaging tests, and sometimes additional laboratory tests. Here’s how a stroke is generally diagnosed:
1. Clinical Evaluation
- History and Symptoms: A healthcare provider will ask about the onset of symptoms, their nature, and duration. Common symptoms include sudden weakness or numbness, difficulty speaking or understanding speech, vision problems, dizziness, and severe headache.
- Physical Examination: The doctor will check for signs of neurological impairment, such as weakness or numbness on one side of the body, difficulty with coordination, and problems with speech or vision.
2. Neurological Examination
- The healthcare provider will perform a detailed neurological examination to assess the patient’s cognitive and physical abilities. This might include testing reflexes, muscle strength, sensation, coordination, and mental status.
3. Imaging Tests
- CT Scan (Computed Tomography): A CT scan of the brain is often the first imaging test performed. It helps to quickly identify whether the stroke is ischemic (caused by a clot) or hemorrhagic (caused by bleeding). A CT scan can also rule out other conditions that may cause similar symptoms.
- MRI (Magnetic Resonance Imaging): An MRI provides a more detailed image of the brain than a CT scan and can detect smaller areas of brain tissue that have been damaged by a stroke, especially in the early stages.
- CT Angiography (CTA) or MR Angiography (MRA): These imaging techniques involve injecting a contrast dye into the blood vessels to visualize the arteries in the brain and neck. They help to identify blockages or abnormalities in the blood vessels.
4. Blood Tests
- Blood tests may be done to check for risk factors like high blood sugar, clotting disorders, infection, or other conditions that could mimic stroke symptoms.
- Coagulation Tests: These tests measure how well the blood is clotting and can help identify bleeding disorders that might contribute to hemorrhagic stroke.
- Blood Sugar Test: Hypoglycemia (low blood sugar) can mimic stroke symptoms, so checking blood sugar levels is essential.
5. Electrocardiogram (ECG)
- An ECG is often done to check for heart problems, such as atrial fibrillation, which is a common cause of ischemic stroke.
6. Echocardiogram
- This ultrasound of the heart can help detect sources of clots that may have traveled from the heart to the brain, especially in cases of ischemic stroke.
7. Carotid Ultrasound
- This test uses sound waves to create images of the carotid arteries in the neck to check for blockages or narrowing that could reduce blood flow to the brain.
8. Cerebral Angiography
- In some cases, a more detailed imaging test called cerebral angiography might be done. This involves injecting a contrast dye into the arteries and taking X-rays to see the blood flow in the brain’s blood vessels in more detail.
9. Lumbar Puncture
- If a hemorrhagic stroke is suspected and imaging tests do not provide a clear answer, a lumbar puncture (spinal tap) might be performed to check for blood in the cerebrospinal fluid.
10. Additional Tests
- In certain cases, other tests might be ordered to assess the patient’s overall health and look for underlying conditions that could increase the risk of stroke.
Emergency Response
Given that a stroke is a medical emergency, the priority is to act quickly. If a stroke is suspected, emergency medical services (EMS) should be contacted immediately, and the patient should be taken to a hospital equipped to handle stroke cases, ideally a stroke center, where rapid diagnosis and treatment can be provided. The speed of diagnosis and treatment is critical in minimizing brain damage and improving outcomes.
The symptoms of a stroke, including a mini-stroke (Transient Ischemic Attack, or TIA), can be sudden and severe. Here’s a comprehensive list of common symptoms to watch for:
Common Stroke Symptoms (FAST)
- Face Drooping: One side of the face may droop or become numb. This is often noticeable when the person tries to smile.
- Arm Weakness: One arm may become weak or numb. If the person tries to raise both arms, one arm may drift downward.
- Speech Difficulty: Speech may become slurred, or the person may have difficulty speaking or understanding others.
- Time to Call Emergency Services: If any of these symptoms are observed, it’s crucial to call emergency services immediately.
Additional Stroke Symptoms
- Sudden Numbness or Weakness: This can occur in the face, arm, or leg, especially on one side of the body.
- Sudden Confusion: The person may suddenly have trouble understanding speech or expressing themselves.
- Sudden Vision Problems: This may include blurred vision, double vision, or loss of vision in one or both eyes.
- Sudden Trouble Walking: The person may experience dizziness, loss of balance, or lack of coordination.
- Sudden Severe Headache: This may come on without a known cause and is often described as the worst headache of one’s life.
- Sudden Difficulty Swallowing: Also known as dysphagia, difficulty swallowing can occur during a stroke.
- Sudden Nausea or Vomiting: These symptoms can accompany other signs of a stroke, especially if they appear suddenly.
- Sudden Numbness or Tingling: A sensation of numbness or tingling, particularly on one side of the body, can be a sign of a stroke.
- Sudden Dizziness or Vertigo: A person may feel like the room is spinning or that they are losing their sense of balance.
Mini-Stroke (TIA) Symptoms
- Similar to Stroke Symptoms: A TIA has the same symptoms as a stroke but is temporary and typically lasts only a few minutes to a few hours.
- Sudden Onset: The symptoms of a TIA come on suddenly, just like a full stroke.
- Transient Nature: The symptoms may resolve completely within 24 hours, often within minutes, without causing permanent damage. However, it’s a serious warning sign and requires immediate medical attention.
Atypical Symptoms (Less Common)
- Sudden Confusion or Disorientation: The person may suddenly appear confused, have trouble understanding what is happening, or be unable to follow simple instructions.
- Sudden Changes in Behavior: Unusual mood swings, agitation, or sudden depression may occur.
- Sudden Fatigue or Weakness: A feeling of extreme fatigue or weakness can sometimes be a symptom of a stroke.
- Difficulty Breathing: In rare cases, shortness of breath or difficulty breathing may be associated with a stroke.
Recognizing these symptoms early and acting quickly can be crucial in minimizing the damage caused by a stroke or TIA. If you or someone else experiences any of these symptoms, it’s important to seek emergency medical attention immediately.
Several risk factors can significantly increase the likelihood of having a stroke. These risk factors can be broadly categorized into modifiable (those that can be changed or managed) and non-modifiable (those that cannot be changed). Here’s a comprehensive list:
Modifiable Risk Factors
- High Blood Pressure (Hypertension):
- The leading cause of stroke, high blood pressure can damage blood vessels, making them more likely to rupture or become blocked.
- Smoking:
- Smoking damages blood vessels, raises blood pressure, and makes blood more likely to clot, all of which increase stroke risk.
- Diabetes:
- People with diabetes have a higher risk of stroke due to the damage high blood sugar can cause to blood vessels.
- High Cholesterol:
- High levels of cholesterol can lead to the buildup of plaques in the arteries, increasing the risk of blockages that can cause a stroke.
- Obesity:
- Excess body weight increases the risk of high blood pressure, diabetes, and high cholesterol, all of which are stroke risk factors.
- Physical Inactivity:
- A sedentary lifestyle contributes to obesity, high blood pressure, diabetes, and high cholesterol, all of which increase stroke risk.
- Poor Diet:
- Diets high in saturated fats, trans fats, cholesterol, and sodium can contribute to high blood pressure, high cholesterol, and obesity, all risk factors for stroke.
- Excessive Alcohol Consumption:
- Heavy drinking can raise blood pressure, increase the risk of atrial fibrillation, and lead to stroke.
- Atrial Fibrillation:
- This irregular heartbeat increases the risk of stroke by allowing blood to pool and form clots in the heart, which can then travel to the brain.
- Drug Use:
- The use of certain drugs, particularly stimulants like cocaine, can increase the risk of stroke by raising blood pressure and causing blood vessels to constrict.
- Stress:
- Chronic stress can lead to high blood pressure and other unhealthy behaviors that increase stroke risk.
- Sleep Apnea:
- This condition, characterized by pauses in breathing during sleep, can lead to high blood pressure and other cardiovascular problems, increasing the risk of stroke.
- Hormone Therapy:
- Certain hormone therapies, including birth control pills and hormone replacement therapy, can increase the risk of stroke, especially in women who smoke or have other risk factors.
- Unhealthy Sleep Patterns:
- Both too little and too much sleep have been linked to an increased risk of stroke.
- Carotid Artery Disease:
- Narrowing of the carotid arteries, which supply blood to the brain, can lead to stroke.
Non-Modifiable Risk Factors
- Age:
- The risk of stroke increases with age, particularly after age 55.
- Gender:
- Men have a higher risk of stroke than women, but women are more likely to die from a stroke.
- Family History:
- A family history of stroke or other cardiovascular diseases increases the risk of stroke.
- Previous Stroke or Transient Ischemic Attack (TIA):
- Having had a previous stroke or TIA increases the risk of having another stroke.
- Race and Ethnicity:
- Certain racial and ethnic groups, such as African Americans and Hispanics, have a higher risk of stroke than others, often due to a higher prevalence of high blood pressure, diabetes, and obesity.
- Genetics:
- Some genetic conditions, such as sickle cell disease, can increase the risk of stroke.
Other Risk Factors
- Heart Disease:
- Conditions such as coronary artery disease, heart valve defects, and heart failure can increase the risk of stroke.
- Peripheral Artery Disease (PAD):
- Narrowing of the arteries in the limbs can indicate widespread atherosclerosis, increasing the risk of stroke.
- Inflammatory Conditions:
- Conditions like lupus and rheumatoid arthritis can cause inflammation in blood vessels, increasing stroke risk.
- Blood Disorders:
- Certain blood disorders, like polycythemia and thrombocythemia, which cause the blood to be thicker or more prone to clotting, can increase the risk of stroke.
Managing the modifiable risk factors through lifestyle changes, regular medical check-ups, and, when necessary, medications can significantly reduce the likelihood of having a stroke.
Making certain lifestyle changes can significantly reduce the risk of stroke. Here’s a list of recommended changes to help prevent stroke:
1. Manage Blood Pressure
- Monitor Regularly: Keep blood pressure within a healthy range (generally below 120/80 mm Hg). Regularly monitor your blood pressure at home and with your healthcare provider.
- Medications: If necessary, take prescribed medications to control high blood pressure.
2. Adopt a Healthy Diet
- Eat a Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Reduce Sodium Intake: Limit salt consumption to help control blood pressure.
- Limit Saturated Fats and Trans Fats: These can raise cholesterol levels and increase stroke risk.
- Increase Fiber Intake: Consuming more fiber can help reduce cholesterol and improve heart health.
- Moderate Alcohol Consumption: If you drink alcohol, do so in moderation—no more than one drink per day for women and two for men.
3. Exercise Regularly
- Aim for Consistency: Engage in moderate-intensity exercise (like brisk walking, swimming, or cycling) for at least 150 minutes per week.
- Incorporate Strength Training: Include muscle-strengthening activities at least two days a week.
4. Maintain a Healthy Weight
- Weight Loss: If overweight, work on losing weight gradually through a combination of healthy eating and regular physical activity.
- Monitor BMI and Waist Circumference: Keep track of body mass index (BMI) and waist circumference as indicators of healthy weight.
5. Quit Smoking
- Seek Help: Use smoking cessation aids and support programs if needed.
- Avoid Secondhand Smoke: Stay away from environments where you might be exposed to secondhand smoke.
6. Limit Alcohol Consumption
- Moderation is Key: Stick to recommended limits—up to one drink per day for women and two for men.
- Avoid Binge Drinking: Binge drinking increases blood pressure and the risk of atrial fibrillation, both of which can lead to stroke.
7. Control Diabetes
- Monitor Blood Sugar: Keep blood sugar levels under control through diet, exercise, and medications if necessary.
- Regular Check-ups: Work closely with your healthcare provider to manage diabetes effectively.
8. Manage Cholesterol Levels
- Diet and Exercise: A healthy diet and regular exercise can help manage cholesterol levels.
- Medications: If prescribed, take cholesterol-lowering medications as directed.
9. Limit Stress
- Practice Relaxation Techniques: Engage in activities like meditation, yoga, deep breathing exercises, or hobbies that help reduce stress.
- Manage Work-Life Balance: Try to balance work and personal life to reduce overall stress levels.
10. Get Adequate Sleep
- Aim for 7-9 Hours: Ensure you get sufficient, quality sleep each night.
- Address Sleep Disorders: Seek treatment for sleep disorders like sleep apnea, which can increase stroke risk.
11. Stay Hydrated
- Drink Plenty of Water: Staying hydrated helps maintain overall health and can prevent conditions that might increase stroke risk, like dehydration-induced high blood pressure.
12. Avoid or Manage Chronic Conditions
- Monitor and Manage Health: Keep conditions like atrial fibrillation, heart disease, and carotid artery disease under control with regular medical care.
13. Limit Caffeine Intake
- Moderate Consumption: While moderate caffeine consumption is generally safe, excessive intake can raise blood pressure.
14. Regular Check-Ups
- See Your Doctor Regularly: Regular health check-ups can help catch and manage conditions that increase stroke risk, such as high blood pressure, diabetes, and high cholesterol.
15. Be Aware of Stroke Symptoms
- Act Fast: Recognize the symptoms of a stroke (using the acronym FAST: Face drooping, Arm weakness, Speech difficulty, Time to call emergency services) and seek immediate medical attention if they occur.
Implementing these lifestyle changes can significantly lower your risk of stroke and contribute to overall better health.

